What are the risks of not breastfeeding?
Breastfeeding is a biological norm. All mammals are biologically designed to nourish their young through breastfeeding. It is only normal. When there is a deviation from the normal, there may be consequences. These consequences occur due to suboptimal or no breastfeeding.
Not breastfeeding can affect the health of both – the baby and the mother – adversely. A meta-analysis by the Agency for Healthcare Research and Quality reviewed this evidence in detail. It was found that “for infants, not being breastfed is associated with an increased incidence of infectious morbidity, as well as elevated risks of childhood obesity, type 1 and type 2 diabetes, leukemia, and sudden infant death syndrome (SIDS). For mothers, failure to breastfeed is associated with an increased incidence of premenopausal breast cancer, ovarian cancer, retained gestational weight gain, type 2 diabetes, myocardial infarction, and metabolic syndrome.” [ source: Alison Stuebe, MD, MSc, Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, the University of North Carolina at Chapel Hill, Chapel Hill, NC ]
Health Risks of Not Breastfeeding:
These can be classified into two categories.
A. Health risks to the baby
B.Health risks to the mother
A. Some of the health risks of not breastfeeding to the baby are as follows:
1.Increased risk of infectious morbidity –
Formula-fed infants are at a higher risk for infectious morbidity as compared to breastfed infants in the first year of life. There are innate immune factors in breast milk that provide protection against infections. In addition, the plasma cells in the mother’s body produce IgA antibodies specific to the antigens in the mother and infant’s immediate surroundings. These antibodies are transferred through breast milk, providing additional protection to the baby. Breastfeeding provides protection against many infections including common respiratory diseases like influenza, pneumonia as well as intestinal diseases like cholera, diarrhea etc. Breastfeeding also reduces the risk of HIV transmission from the mother and provides innate immunity against viruses causing herpes etc.
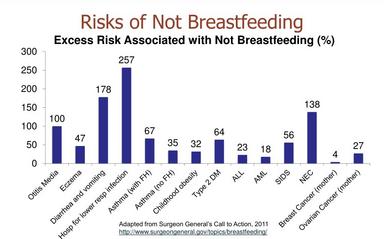
2. Otitis Media (Ear Infections) –
Approximately 44% of babies get ear infections at least once in the first year. For formula-fed infants, this risk is doubled as compared to those who are exclusively breastfed for more than 3 months.
3.Lower Respiratory Tract Infection –
Research has found that infants who did not breastfeed faced a 3.6-fold increased risk of hospitalization in the first year of life as compared to those who breastfed for more than 4 months.
4.Gastrointestinal Infection –
Many studies have suggested that formula-fed babies face an increased risk of gastroenteritis and diarrhea. This also includes combi-fed babies.
5.Necrotizing Enterocolitis (NEC) –
This is a devastating disease affecting preterm babies wherein the wall of the intestine is invaded by the bacteria causing infection and could lead to the destruction of the wall. This is a serious infection having a case fatality rate of 15%. Not being breastfed is associated with a 2.4-fold risk of NEC.
6.Obesity and Diabetes –
a. Studies suggest that babies who are fed formula in infancy are 1.1 to 1.3 times more likely to become obese as children compared to exclusively breastfed babies.
b. A 1.6-fold risk of developing Type 2 Diabetes is also associated with being fed formula in infancy.
c. Breastfeeding for less than 3 months is associated with a 1.2 to 1.4-fold increased risk of developing Type 1 Diabetes.
7.Childhood Leukaemia –
a. Meta-analyses of studies suggest a 1.3-fold higher risk of acute lymphoblastic leukemia among formula-fed children compared with children who were breastfed less than 6 months.
b. Studies have also found a 1.2-fold higher risk of acute myeloid leukemia among formula-fed infants compared with infants breastfed more than 6 months.
8.Cognitive Development –
Several studies have reported lower IQ scores among formula-fed children as compared to those who were breastfed. Studies have also found evidence of developmental differences with shorter durations of breastfeeding.
9.Sudden Infant Death Syndrome (SIDS) –
Studies suggest that formula feeding is associated with a 1.6 to 2.1-fold increased chance of SIDS as opposed to breastfeeding.
10.Other risks –
Multiple studies (some, with mixed results) have suggested that formula-fed babies are at an increased risk of developing allergies. This includes Asthma. Formula-fed babies are also at an increased risk to develop Atopic Dermatitis (Eczema). Some studies have indicated an increase in risk for cardiovascular disease, including higher blood pressure and less favorable lipid profiles in adulthood when fed formula in infancy. However, the literature is mixed.
B. Some of the health risks of not breastfeeding to the mother are as follows:
- Breast Cancer –
An inverse relation has been found between breastfeeding and premenopausal breast cancer risk. This means that the longer the duration of breastfeeding, the lesser the risk of developing breast cancer before menopause. A meta-analysis found that each year of breastfeeding amounted to a 4.3% reduction in risk of invasive breast cancer.
2. Ovarian Cancer –
Never having breastfeeding has been associated with a 1.3-fold higher risk of ovarian cancer as compared to ever having breastfed.
3. Retention of gestational weight gain –
Studies have indicated that exclusive breastfeeding helps in losing the weight gained during pregnancy. So, not breastfeeding increases the odds of retaining the gestational weight gain.
4. Diabetes –
The risk of developing Type-2 Diabetes has been found to be 1.7-fold higher in women who have never breastfed as compared to those who have breastfed for at least 2 years or more.
5. Osteoporosis –
Studies have found a significantly lower prevalence of osteoporosis (8%) in women who had breastfed as compared to those who did not breastfeed (19%).
6. Other risks –
Studies have found a 10% to 20% higher risk of diabetes, hyperlipidemia, and cardiovascular disease among women who had never breastfed compared with those who breastfed for 13 to 23 months.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2812877/
https://kellymom.com/nutrition/milk/infant-formula/
http://www.tensteps.org/pdf/21dangers-jun2012.pdf
https://cdn.mdedge.com/files/s3fs-public/issues/articles/70360_main_26.pdf
https://www.bones.nih.gov/health-info/bone/bone-health/pregnancy#
Wish to speak with a member of our team who is a certified lactation professional and also an experienced breastfeeding mother, click on this link.
Medical Advice Disclaimer
THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Disclaimer
We understand and acknowledge that parents and babies can be of various genders on a spectrum of LGBTQI+. Families come in diverse flavours. However, in our articles, for the sake of simplicity and convenience, we will be referring to the breastfeeding parent as the mother and using the female pronouns- ‘she’ and ‘her’ for babies. Babies can be nourished and nurtured in different ways and while we have used the terms breastfeeding and nursing, we recognize that parents can opt to chest feed or finger feed.
We don’t have conflicts of interest and declare, and we are compliant with the WHO code of marketing of breastmilk substitutes and the IMS act.
In case you find any information on this website that needs to be updated, please write to us at info@bsim.org.in






